Virtual care was finding a place in the healthcare industry and saw explosive growth in recent years—well before the COVID-19 pandemic. But it’s safe to say that it transformed healthcare seemingly overnight when the U.S. government put lockdown and social distancing mandates in place in 2020.
There’s no denying that virtual care provides patients greater convenience, more access to physicians and specialists (especially in rural areas), and lower healthcare costs.
However, as with any new technology, virtual care has been shown to have its advantages and disadvantages. Some people remain doubtful of the extent to which virtual care delivers positive outcomes.
Understanding the benefits of virtual care and its limitations is essential for organizational leaders and HR professionals to grasp. As your employees’ provider of healthcare benefits, you can better educate your workforce on their benefits and the landscape of virtual health—helping them utilize virtual care options when appropriate and recognizing when in-person care is best.
What is virtual care?
Many experts in the industry use the terms telehealth, telemedicine and virtual care interchangeably, and others seem to have different definitions for them.
This article focuses on the benefits of a broader definition of virtual care:
Virtual care encompasses the various ways doctors can provide healthcare services to patients through digital tools such as video calls, phone calls, instant messaging, or remote monitoring, which may replace or accompany in-person appointments with a healthcare provider.
Virtual care can take many different forms. Here are several ways that health care providers can connect digitally with their patients and their health data:
- Synchronous: Real-time interaction via telephone or live audio-video using a smartphone, tablet or computer.
- Asynchronous: A way to interact with a provider that securely stores messages, images and data that can be read, interpreted or responded to later.
- Remote patient monitoring: The use of technology to transmit accurate patient data to a healthcare provider, like at-home blood pressure or glucose monitoring devices.
Virtual Healthcare Trends and Statistics
According to a Doximity state of telemedicine report, virtual health visits increased drastically in the first months of the pandemic. There was a 57% increase in the number of individuals who opted to use them.
A report by McKinsey & Company puts the number of those using virtual health visits even higher, with healthcare providers seeing 50 to 175 times the number of patients through virtual visits than they averaged before the pandemic began.
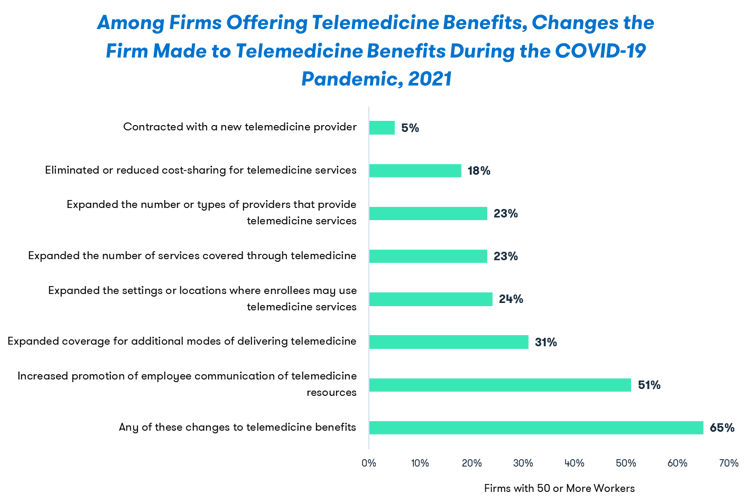
To accommodate this shift, employers are also making changes to their benefits plans. Take a look at the changes reported by the Kaiser Family Foundation Employer Health Benefits Survey, 2021:
Plus, widespread adoption of virtual care could shift $250 billion of health care spending from in-person to virtual care services and, deployed strategically and comprehensively, could save the U.S. $46 billion in healthcare spending. Thus, harnessing digital innovation has become a priority for most benefits buyers in 2020 and beyond.
The Benefits of Virtual Care
Virtual care visits are more convenient than most trips to the doctor—and may increase healthcare utilization.
Like most other industries that have moved increasingly towards digital services, convenience for both parties is the most apparent factor in the future reception of telehealth. Driving to the doctor's office, waiting in the waiting room and waiting again in the exam room for a seven-minute visit hardly seems desirable when you could get the same level of care from your car on your lunch break.
Too often, an individual will miss out on regular checkups because they can’t fit appointments into their busy life or take time off work. In one study, 16% of people who completed a virtual care visit said they would have “done nothing” as an alternative to a telemedicine visit, highlighting that healthcare utilization may increase when virtual care is an option.
Virtual care has shown to be more cost-effective by diverting patients away from more costly care settings—like the emergency room.
Virtual consultations can save a person an unnecessary trip to the emergency department by enabling them to check with a healthcare provider to find out the most appropriate place to seek care is for their situation.
This can also significantly lower overall costs since a trip to the emergency room is considerably more expensive than a virtual care visit. One study on virtual care found that each avoided emergency department garnered cost savings ranging from per visit.
Virtual options increase access in rural areas.
Another reason for the escalation in virtual care services is the decline in traditional access to healthcare in rural areas.
Nearly 20% of the U.S. population live in rural areas, but less than 8% of doctors and healthcare professionals practice there.
With virtual options, if a patient can’t find the service they need locally, they have the option of connecting with a specialist through any device with an internet connection. This enables individuals and families to receive healthcare and access to prescriptions without traveling long distances.
Virtual care can improve health outcomes.
Not only can virtual care provide a return on investment in a financial sense, but it can also offer a “return on health.” There are many real-world examples of virtual care applications that show:
- Improved access to highly qualified specialty care providers for faster and more accurate diagnoses and treatments
- Improved medication adherence, which leads to fewer clinical problems and complications
- Decreased hospital admissions
- Increased patient satisfaction scores
Virtual health care services can reduce strain on the healthcare system.
The reason virtual care became prevalent during the COVID-19 pandemic is also a benefit of virtual care. Virtual care allows providers to improve their team’s efficiency and meet the needs of more patients while reducing wait times for patients. It can also reduce healthcare employee burnout by decreasing the workload for their staff. Less burnout in the healthcare system means better continuity and quality of care for patients everywhere.
Telehealth can increase access to specialty care, regardless of the patient or provider’s location.
Over time, technology has freed us from the bounds of geography, seen through the films we watch, the radio we listen to, who our friends are and where we work. We’ve been able to choose the best options for us in so many facets of life, and now the healthcare industry is simply following suit.
“Historically, we’ve sought care based on our zip code, considering ‘What clinics can we attend?’ and ‘What doctors can we see within a 30-minute drive?’ We’re expecting them, many times, to be a Jack of all trades versus in the telemedicine world - you’re starting to see care teams assembled based on the diagnosis. So as a person with diabetes, you’re going to have people who work with diabetics all day every day and have the latest, greatest intelligence, and they may be 300 miles from you and you don’t know or care.” – Jim Pshock, Bravo CEO.
The Potential Downsides of Virtual Healthcare
Virtual options can impact an individual’s continuity of care.
Suppose the healthcare provider you connect with virtually is not your usual primary care physician or specialist. In that case, they may not have access to your comprehensive medical record, which can increase the risk of misdiagnosis, medical errors, or inappropriate treatment. This lack of information goes both ways: if your regular provider doesn’t have notes from the virtual visit, they could miss important information about your health, and you may not get the appropriate care.
Virtual care requires a person to have both internet access and a device and a degree of tech literacy.
There’s simply no way around the fact that virtual visits require the internet. And nearly one in four households—equating to 27.6 million U.S. households—don’t have the internet at home.
Additionally, virtual services heavily rely on a good online connection that not everyone has. Add to this problem that around 15% of Americans don’t own a smartphone. Unless a patient can afford a reliable device and internet and use them properly, they won’t have access to virtual care.
Virtual care cannot replace every in-person service.
Of course, specific exams and any medical procedures and surgeries require patients to be physically present with a health care professional. However, significant strides in the digital health space have made at-home monitoring for diabetes prevention and management, cardiac rehabilitation, pregnancy and many other conditions much more accessible and cost-effective for patients and the health system.
Reimbursement and regulations are still significant barriers to virtual care.
Unfortunately, telemedicine is not “equal” to in-person care in the eyes of many insurance companies. While Medicare and some private health plans have taken voluntary steps to increase access to virtual care options during the pandemic, 49% of insured adults get health insurance from their employer, not requiring coverage for virtual care services.
In a significant step forward for the future of virtual care, the House of Representatives submitted a bipartisan bill that ensures all patients, including those covered by an employer-funded health plan, permanently have telehealth coverage. The American Medical Association sent a letter in support of the bill, stating access to telehealth during the pandemic and beyond is “a vital lifeline for millions of Americans, proving particularly important for the elderly, individuals with chronic conditions and patients with special mental health needs.”
When should you use virtual care instead of making an in-person doctor’s appointment?
When no physical exams need to occur, and the reason to speak with a health care professional is to discuss one’s lifestyle or test results, virtual doctor’s visits are a no-brainer. There are also significant benefits to incorporating virtual care elements into your employee wellness program, particularly in employee health coaching, chronic condition management and mental health benefits.
However, it’s essential to know when to visit your healthcare provider versus schedule a telehealth appointment and make sure you understand what is covered by your insurance plan.
Here are several ways virtual care can be used effectively for employees when covered by insurance and incorporated in your benefits plan:
- Screen patients for COVID-19 symptoms and refer them to get tested and treated, if necessary
- Access primary care providers and specialists, including mental and behavioral health, for chronic health conditions and medication management
- Provide coaching and support for patients managing chronic health conditions, including weight management and nutrition counseling
- Participate in physical therapy, occupational therapy and other modalities as a hybrid approach to in-person care for optimal health
- Monitor clinical signs of certain chronic medical conditions (e.g., blood pressure, blood glucose, other remote assessments)
- Engage in case management for patients who have difficulty accessing care (e.g., those who live in very rural settings, older adults, those with limited mobility)
- Follow up with patients after hospitalization
- Deliver advance care planning and counseling to patients and caregivers to document preferences if a life-threatening event or medical crisis occurs
- Provide non-emergent care to residents in long-term care facilities
How Virtual Care Can Integrate with Wellness Initiatives and Benefit Your Workforce
Perhaps the most crucial way virtual care can help improve the overall health of your workforce is by making care more accessible to those within the organization—especially for those with or at risk for chronic conditions.
Talk with your benefits consultant about how you can incorporate virtual care into your benefits plan to serve employees with convenient and effective healthcare solutions.
And, if you’re ready to get your people back on track with preventive care that can reduce costs and health risks in your organization, let’s talk. Bravo can help your people prioritize preventive care and health improvement by administering incentives that steer employees to a primary care provider, and even reward them for making changes recommended by their doctor.
Eager to learn more about virtual care and how consumers and the healthcare industry will spend much of the future navigating between the two? Be sure to listen to our podcast episode, Is the Future of Healthcare Virtual?


